Every winter here in Texas, our phones light up with the same question: “I feel terrible, but I’m not sick. Is this normal?”
You wake up congested. Your head feels fuzzy. You’re exhausted even though you slept. You pop an antihistamine — it helps a little, but not enough. You wonder if certain foods are making it worse. Nothing adds up.
If this sounds familiar, you’re not alone. And you’re not imagining it.
What you’re experiencing could be seasonal allergies (hello, cedar fever), histamine intolerance, or — most likely — a combination of both. Understanding the difference matters because the right approach depends on why your body is reacting.
What Is Histamine (and Why Do We Need It?)
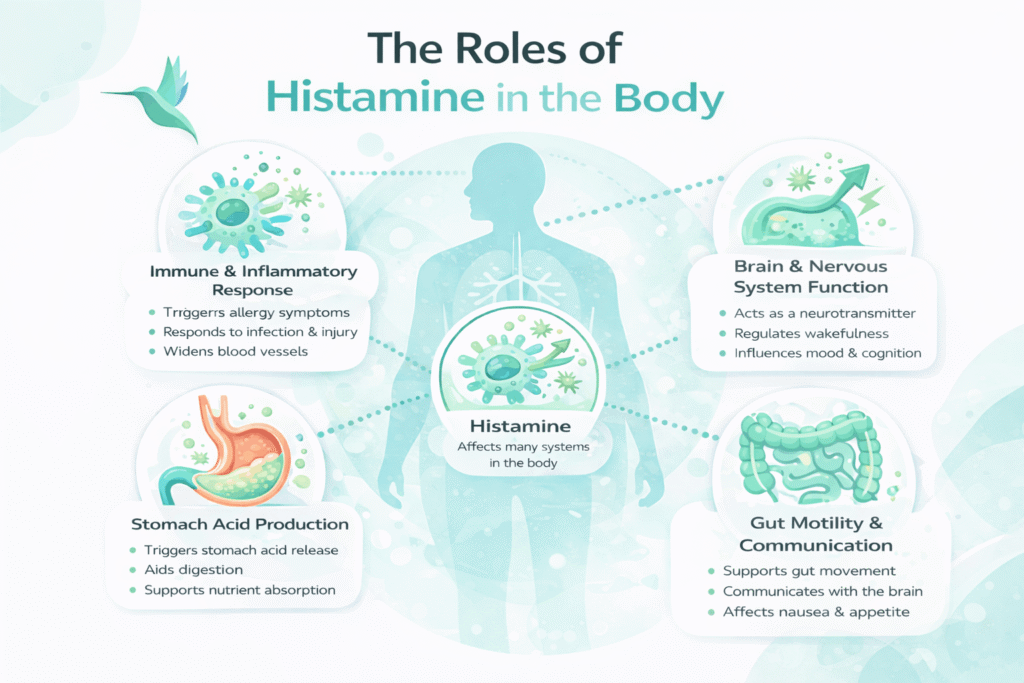
Histamine isn’t the enemy — it’s actually essential for your body to function. This natural chemical plays key roles in:
- Immune defense (fighting off infections and allergens)
- Digestion (stimulating stomach acid production)
- Brain function (neurotransmitter signaling)
- Inflammatory responses (healing injuries)
Think of histamine as your body’s alarm system. In normal amounts, it protects you. Problems arise when histamine accumulates faster than your body can break it down.
This is what integrative medicine practitioners call histamine intolerance — though it’s worth noting that mainstream medicine is still debating whether this is a distinct diagnosis or a symptom of other underlying conditions.
True Allergies vs. Histamine Intolerance: What's Actually Different?
True Allergies
Allergies involve a specific immune response to an identifiable trigger — like cedar pollen, dust mites, or mold.
Classic allergy symptoms:
- Sneezing and nasal congestion
- Itchy, watery eyes or throat
- Runny nose with clear mucus
- Symptoms follow a predictable pattern (worse on high-pollen days)
- Standard allergy testing can identify triggers
Important for Texans: Cedar pollen season typically peaks in mid-January, and the sheer quantity of pollen can overwhelm even people who don’t normally have allergies.
Learn more about our in-clinic allergy testing HERE.
Histamine Intolerance
Histamine intolerance occurs when multiple factors stack up, pushing your total histamine “bucket” past your body’s ability to process it.
These factors might include:
- Environmental allergens (like that infamous cedar pollen)
- High-histamine foods (aged cheese, fermented foods, wine, leftovers)
- Chronic stress or poor sleep
- Gut inflammation or digestive issues
- Hormonal fluctuations
- Recent illness
- Certain medications that block DAO (the enzyme that breaks down histamine)
Symptoms feel less predictable and more widespread:
- Headaches or migraines
- Flushing or unexplained skin reactions
- Digestive discomfort (bloating, diarrhea)
- Brain fog and difficulty concentrating
- Fatigue that doesn’t match your activity level
- Symptoms that worsen with stress or vary day-to-day
The confusing part: These symptoms can feel random because they don’t always correlate with a single trigger.
Why Winter in Texas is a Perfect Storm for Histamine

If you’ve noticed you feel worse every winter, there’s a reason. Texas winters create a unique combination of histamine stressors:
- Sky-high cedar pollen levels — Central Texas experiences some of the highest concentrations in the nation
- More indoor time — Increased exposure to dust, mold, and pet dander
- Post-holiday disruption — Irregular sleep, travel stress, and dietary changes
- Stress-induced immune dysregulation — Your nervous system affects histamine release
- Gut health challenges — Winter illnesses, antibiotics, and dietary changes impact DAO production
Even if you “never had allergies before,” this combination can push your system over the edge.
The Real Controversy: Is Histamine Intolerance Even Real?
Here’s what you need to know: A 2023 study found that most people who believed they had histamine intolerance actually had other conditions causing similar symptoms. The medical community is divided on whether histamine intolerance is a distinct diagnosis or a symptom of underlying issues like:
- Food allergies or sensitivities
- Small intestinal bacterial overgrowth (SIBO)
- Mast cell activation syndrome
- Irritable bowel syndrome (IBS)
- Medication side effects
What this means for you: The label matters less than understanding what’s happening in YOUR body. Our integrative approach looks at the full picture rather than forcing your symptoms into a single diagnosis.
How West Holistic Medicine Figures Out What's Going On
We don’t play the guessing game with your health. Instead, we investigate from multiple angles:
Working With Our Integrative Physicians
Our integrative approach examines:
- Your total inflammatory load and how your body processes histamine
- Gut health markers and immune system signaling
- Nutritional factors (vitamin deficiencies, DAO cofactors)
- Stress and nervous system regulation
- Why symptoms persist even when allergy tests come back normal
The goal: Understand why your body is reacting, not just what it’s reacting to.
Working With Our Family Nurse Practitioner
For more straightforward allergy concerns, our FNP-c can:
- Determine if standard allergy testing is appropriate
- Identify environmental triggers
- Recommend evidence-based treatments
- Clarify when conventional allergy approaches make sense
- Guide you toward holistic allergy support when appropriate
Read more about our Integrative Physicians HERE.
The Goal Isn't Restriction — It's Building Resilience
Let’s be clear: we’re not here to put you on an endless elimination diet or keep you dependent on antihistamines forever.
Our approach focuses on:
- Reducing your total inflammatory burden (not just one factor)
- Supporting your body’s natural histamine processing (especially DAO enzyme function)
- Calming immune system overactivity (addressing root causes)
- Helping you feel stable and less reactive (rebuilding resilience)
When your body feels supported, symptoms often improve naturally — without extreme restrictions.
When Should You Consider Professional Support?
Consider scheduling an evaluation if:
✓ Over-the-counter antihistamines only partially help
✓ Your symptoms feel inconsistent or difficult to explain
✓ Food reactions seem random or unpredictable
✓ Stress clearly makes your symptoms worse
✓ You’ve tried multiple approaches without lasting relief
✓ You’re tired of feeling like you’re “just dealing with it”
You Don't Have to Choose Between Conventional and Holistic Care
At West Holistic Medicine, we bridge both worlds. Whether your symptoms are straightforward seasonal allergies or a more complex histamine picture, we’ll create a personalized, root-cause-focused plan.
New Patients: Please fill out a registration form to schedule your first appointment
Returning Patients: Log in to your online portal to book
Or give our office a call at 512-814-0148, and we’ll be happy to help!
